
When Winter Darkness Affects Mental Health
- Seasonal Affective Disorder (SAD) is a form of major depressive disorder that follows a seasonal pattern, most commonly beginning in fall or winter due to reduced daylight and circadian rhythm disruption.
- Winter blues and Seasonal Affective Disorder are not the same.
- The biological cause is measurable – people with SAD have reduced sensitivity to blue light wavelengths, disrupting serotonin production and circadian rhythms
- Light therapy remains the gold standard treatment, with an 80% effectiveness rate, using 10,000 lux light boxes for 30 minutes each morning.
- CBT-SAD provides lasting skills that prevent recurrence more effectively than light therapy alone over multiple years
- Risk factors include being female aged 18-30, having a family history of SAD (13-17% increased risk), and co-occurring ADHD (3x higher risk)
- Prevention is possible by starting light therapy in early September, establishing exercise routines before winter, and working with a clinical psychologist.
- Multiple evidence-based treatments exist, including light therapy, Cognitive-Behavioral Therapy for SAD, medication (SSRIs and Wellbutrin), vitamin D supplementation, and structured lifestyle changes
- The winter blues involve mild, temporary mood changes, while Seasonal Affective Disorder causes persistent depressive symptoms that interfere with daily functioning. SAD is highly treatable with evidence-based options such as light therapy, CBT-SAD, and medication when needed.
- This article is written by Ginny Estupinian, PhD, a board-certified clinical psychologist in Los Gatos who specializes in evidence-based treatment for depression and Seasonal Affective Disorder.
In this article, you’ll learn:
- The difference between winter blues and Seasonal Affective Disorder
- Why winter darkness affects mood and brain chemistry
- Who is most at risk for seasonal depression
- Which treatments are proven to work
- When to seek professional help

Recently, we discussed the end of daylight saving, and on Sunday, December 21, 2025, at 7:03 AM PST, those of us in the Bay Area will begin the Winter Solstice, marking the shortest day and the start of winter.
The winter solstice marks the time of year when the Earth is at its greatest tilt away from the sun. So in the Northern Hemisphere, during our winter solstice, the Earth’s tilt away from the sun creates the shortest day and longest night of the year.
As daylight saving time ended and winter descended across America, many individuals began to feel a bit different. Commonly, people refer to this dip in our mood as the winter blues, winter depression, seasonal depression, and in specific circumstances, medical providers will diagnose this condition as Seasonal Affective Disorder. So do these all mean the same thing? Not exactly. In this article, we will break it down.
What Are The Winter Blues?
It’s important to distinguish between common seasonal mood changes and a serious medical condition. The winter blues are mild, short-term dips in mood and energy that many people feel during the darker months, but they don’t usually interfere with daily life. As I discussed in a previous blog post, this is usually due to minor circadian rhythm shifts and reduced daylight, which affects mood slightly but not dramatically.
How is Seasonal Affective Disorder Different?
Seasonal Affective Disorder (SAD) is more serious. It’s a form of depression that returns each winter and causes significant symptoms such as low mood, fatigue, sleep changes, and loss of interest in normal activities. The key difference is that winter blues are temporary and manageable, while SAD is a diagnosable condition that benefits from professional treatment.
How prevalent is Seasonal Affective Disorder?
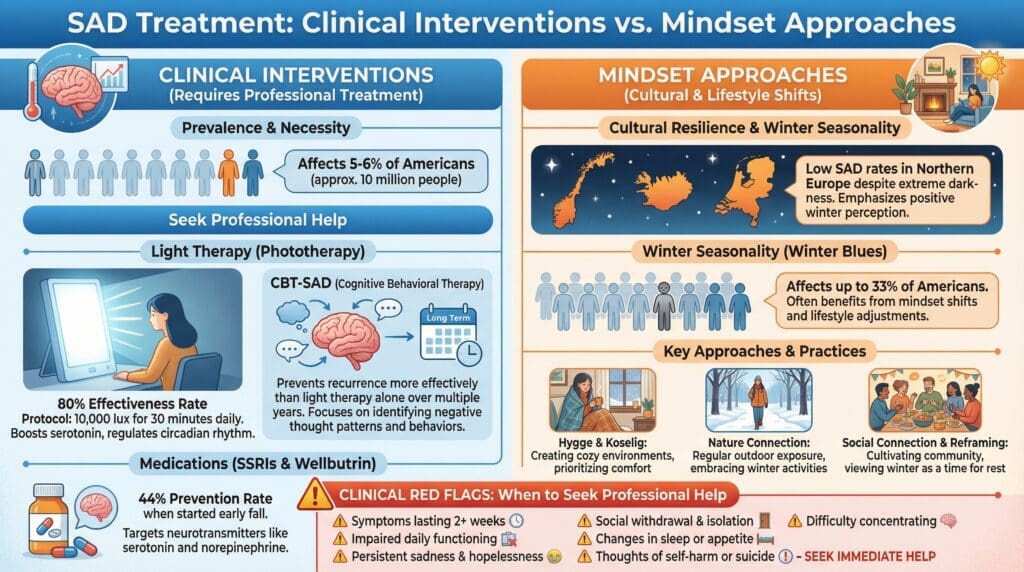
Recent studies report that approximately 10 million Americans, which is roughly 5-6% of the population, experience more than just occasional winter blues. They suffer from Seasonal Affective Disorder (SAD), a condition, as stated above, that follows a predictable seasonal pattern. In the Diagnostic Statistical Manual, it is classified as “Major Depression with Seasonal Pattern”.
First named by Dr. Norman E. Rosenthal and colleagues in 1984, SAD represents a significant mental health challenge that, as Dr. Rosenthal notes, often goes unrecognized despite being “right in front of our noses.” Whether you call it winter depression or use the clinical term SAD, this condition extends far beyond the mild “winter blues” that many experience, though even those less severe seasonal mood changes affect up to one-third of Americans.
SAD is characterized by its cyclical nature and distinct symptom profile, including extreme fatigue, uncontrollable carbohydrate cravings, and hypersomnia. With symptoms lasting approximately 40% of the year and affecting women four times more frequently than men, this seasonal depression causes significant impairment in relationships, employment, and overall quality of life. Understanding that your “winter funk” or “seasonal slump” might actually be a treatable medical condition is the first step toward reclaiming your winters.
The key here is to understand that this form of winter depression is highly treatable, with multiple evidence-based options available to help you thrive year-round, not just survive until spring.
The Science: Why Darkness Messes With Your Brain
Understanding the biology behind SAD helps explain why it’s not just “in your head” and why specific treatments work. The story starts in 1980 when Dr. Alfred Lewy discovered that artificial light could suppress nighttime melatonin production, revolutionizing our understanding of how light affects mood and sleep.
Here’s what happens in your brain during winter: Specialized cells in your retina detect blue light wavelengths, which are abundant in sunlight. These cells send signals through your hypothalamus to various brain regions, including the raphe nuclei, where serotonin is produced. When these cells absorb blue light, your brain’s alertness centers activate, making you feel awake and improving your mood. Winter’s reduced daylight means less exposure to blue light, which triggers a cascade of problems throughout your brain’s mood-regulating systems.
Dr. Kathryn Roecklein’s research at the University of Pittsburgh revealed something fascinating: people with SAD are actually less sensitive to blue light than others, especially during the winter months. This reduced sensitivity appears to be a biological cause of wintertime depression, not just a result of it. In other words, your brain literally needs more light to function properly, but your eyes aren’t as good at processing what little light is available.
The circadian rhythm disruption goes beyond just feeling sleepy at the wrong times. Your internal clock affects hormone production, body temperature, appetite, and numerous other biological processes. When your circadian rhythm is thrown off, it affects multiple neurotransmitter systems. Serotonin levels drop, both because less is produced and because proteins that remove serotonin from your synapses become more active. Dopamine and norepinephrine, which are crucial for motivation and morning energy, also decrease.
Vitamin D
Making matters worse, 41% of U.S. adults have insufficient vitamin D levels, and this deficiency worsens in winter when we get less sun exposure. Vitamin D directly influences serotonin production, creating a double whammy for mood regulation.
Tryptophan
Tryptophan is an essential amino acid found in foods such as turkey, chicken, fish, eggs, cheese, pork, nuts, seeds (sunflower), soy products, oats, and milk. Tryptophan helps make serotonin. Research using tryptophan depletion studies has confirmed that artificially lowering serotonin precursors can trigger depressive symptoms in people who’ve recovered from SAD, proving the crucial role of serotonin in this condition. Below, we will look further into the nutrition that matters.
Who’s at Risk and Why

If you’re a woman in your late twenties or early thirties, you’re in the highest risk group for developing SAD. The condition typically first appears between ages 18 and 30, with 23 being the average age of onset. This timing isn’t coincidental; it often corresponds with major life transitions like finishing college, starting careers, and establishing adult lives, all while trying to maintain some semblance of work-life balance. Women are four times more likely than men to develop SAD, with 45% of women reporting winter mood decline compared to 37% of men.
Family history plays a significant role, too. If you have a parent or sibling with SAD, your risk increases by 13-17%. Scientists have identified specific genetic variations that affect how our bodies process serotonin and, therefore, mood regulation. Some populations, such as Icelanders, appear genetically protected against SAD despite living at extreme northern latitudes. Researchers believe they may have evolved genetic adaptations that actually increase serotonin production during winter months.
Co-occurring Symptoms Make Individuals More Susceptible
The plot thickens when we consider other conditions that often co-occur with SAD. Adults with ADHD are particularly vulnerable, with 27% also experiencing seasonal depression, three times the general population rate. The combination can be especially challenging, as both conditions affect energy, focus, and motivation. If you have diabetes, you’ll need special evaluation before trying light therapy due to potential effects on your eyes. And if you have bipolar disorder, certain SAD treatments could trigger manic episodes, making professional guidance essential.
Treatment That Actually Works
Let There Be Light

Light therapy remains the most effective first-line treatment for SAD, with over 60 clinical studies backing its effectiveness. About 80% of people with SAD respond well to light therapy, especially those with the classic symptoms of oversleeping and carbohydrate cravings.
The key is using the right kind of light at the right time. You need a light box that produces 10,000 lux, which is about 20 times brighter than typical indoor lighting but still much less than a sunny day. The treatment protocol is straightforward: sit about 16-24 inches from the light box for 30 minutes each morning, ideally as soon as you wake up and definitely before noon. Position the light at a 45-degree angle from your eyes. You don’t stare directly at it, but your eyes need to be open for it to work.
Quality matters when choosing a light box. While prices range from $70 to $400, not all products marketed for SAD actually work. Some simply aren’t bright enough, while others might not filter out UV rays properly. Your insurance might even cover part of the cost if you have a SAD diagnosis.
Many people describe the effect as feeling like “a strong cup of coffee without the crash.” The light helps jumpstart your circadian rhythm and increases serotonin production in your brain.
Another recommendation is to combine traditional light therapy with a dawn simulator. Essentially, this is a sunrise alarm clock that gradually brightens your room to help you wake up. This combination addresses both the morning circadian reset and the jarring experience of waking in darkness. Yale has tested products and offers a list of recommendations, and the nonprofit Center for Environmental Therapeutics has a consumer guide to select a light.
CBT-SAD: Changing How You Think About Winter
While light therapy treats the symptoms, Cognitive-Behavioral Therapy for SAD (CBT-SAD) addresses the underlying thought patterns and behaviors that make winter harder than it needs to be. Developed by Dr. Kelly Rohan at the University of Vermont, CBT-SAD has shown remarkable success in preventing SAD recurrence, sometimes even more effectively than light therapy over multiple years.
The therapy works by identifying and changing negative thought patterns about winter. Instead of thinking “I can’t function when it’s dark,” you might reframe it as “I function differently in winter and can adapt.” CBT-SAD also focuses on behavioral activation. This means doing things even when you don’t feel like it, because action can actually change your mood faster than waiting to feel better before taking action.
One of the biggest advantages of CBT-SAD is that once you learn the skills, they’re yours forever. Unlike light therapy, which requires 30 minutes every morning, CBT skills become automatic responses to winter challenges. The therapy typically involves 12-14 sessions and can be done either individually or in groups.
Tips for managing seasonal affective disorder
Thriving Through the Long Nordic Winter

People who live in Northern Europe and above the Arctic Circle have developed effective mental and physical strategies for coping with the annual onset of the winter blues, which can begin as early as October and last well into April.
Rather than dreading the darkness, Nordic cultures emphasize adopting a positive outlook as a survival strategy. Ida Solhaug, an associate professor of psychology at the University of Tromsø, often called the world’s northernmost university, explains that embracing winter and appreciating seasonal change is deeply cultural and essential when daylight is scarce for months at a time.
This mindset is reinforced through daily habits that balance comfort and activity, such as enjoying indoor coziness through hygge while also making time to go outside for traditions like fika, a simple coffee break in the fresh air. Even on cloudy days, brief exposure to daylight and movement can lift mood and energy. As Solhaug puts it, the challenge is to look for light in the darkness, a philosophy captured in a common Nordic saying: there is no such thing as bad weather, only bad clothing.
Lifestyle Changes That Make a Difference
Take in as much daylight as possible. The lack of sun exposure is part of what causes SAD, so soaking up as much as you can may lessen symptoms. Sit by a window or go for a walk during daylight hours. You could even take up a winter sport to get you outside and keep you moving.

Eat healthily. Nutrition plays an important role in managing mood and energy during the darker months, even though you cannot eat your way out of Seasonal Affective Disorder. Maintaining stable blood sugar can make a meaningful difference, so prioritize balanced meals that include protein, especially at breakfast, and keep healthy snacks available when cravings hit.
Comfort food does not have to mean heavy, high-sugar, or high-fat options. With a little creativity, hearty and satisfying meals can also be nutritious and lower in calories. Instead of reaching for cakes or cookies, consider desserts made with seasonal fruits like apples or pears, which offer warmth and sweetness without the crash.
Vitamin D supplementation may also be helpful, particularly since, as mentioned above, nearly half of Americans are deficient, and reduced sunlight during winter can further lower levels. Together, these dietary strategies can help support steadier energy and a more balanced mood throughout the season.
Spend time with your friends and family. Although Seasonal Affective Disorder often pushes people to withdraw, staying socially connected is one of the most effective ways to protect mental health during the darker months. Make social plans that are harder to cancel, such as joining a group fitness class instead of exercising alone or scheduling standing coffee dates or phone calls with friends. Spend intentional time with family and loved ones by snuggling with your kids or pets, sharing a warm drink with a friend, or playing board games together.
These moments of connection help counter isolation and lift mood. It is also important to talk openly about how the season is affecting you and to educate those close to you about SAD, so they can better understand your experience and support you. Think of social connection not as optional, but as essential medicine for your mental well-being.
Stay active. Don’t stay cooped up in your house all winter. Get out and enjoy your community this season. Volunteer, join a local club, go for a walk, or go ice skating with your loved ones to start. Also, if you know you experience SAD year after year, be proactive about planning out a schedule in advance of winter to keep active and engaged with others. Research shows exercise and scheduling pleasant activities can be effective ways to lessen the impact of SAD.
Meditation can be helpful. Emerging research shows that even 10-15 minutes a day can help manage stress and improve emotional regulation during difficult months.
So, the combination of physical activity, light exposure, and fresh air creates a triple benefit for mood. One last thing, remember if you don’t put it on the schedule, it won’t happen. This is especially true when SAD saps your motivation.
Some people find meditation helpful. Dr. Rosenthal, who originally named SAD, now recommends Transcendental Meditation based on his own experience and emerging research. Even 10-15 minutes daily can help manage stress and improve emotional regulation during difficult months.
When Medication Is Necessary
Sometimes, despite light therapy, CBT, and lifestyle changes, medication becomes necessary. This doesn’t mean a person has failed; it means you’re taking your mental health seriously enough to use all available tools. The most commonly prescribed medications for SAD are SSRIs, which help correct the serotonin imbalance underlying SAD symptoms.
Bupropion (Wellbutrin) offers unique benefits for SAD. When started in early fall before symptoms begin, it can prevent SAD episodes in about 44% of cases. This preventive approach is particularly valuable for people with severe SAD who know they’ll struggle come winter.
Medications work best as part of a comprehensive treatment plan rather than a standalone solution. They can provide the boost needed to engage with other treatments, including therapy.
Prevention and Long-Term Management
The key to managing SAD long-term is starting treatment before you need it. Begin light therapy in early September, even if you feel fine.
Establish exercise routines and social commitments while you still have energy, so they’re already habits when motivation drops.
Building a support team is essential. This might include a primary care doctor, a psychologist trained in SAD treatment, and friends or family who understand your condition.
Regular check-ins help catch early warning signs and adjust treatment as needed. Many people find SAD-specific support groups helpful, whether in-person or online.
Creating sustainable strategies means being realistic about what you can maintain. Maybe you can’t commit to 30 minutes of light therapy every single morning, but you could do 20 minutes most days. Perhaps a full gym workout feels impossible, but a 10-minute walk is doable. Small, consistent actions often work better than ambitious plans that fall apart by November.
Track your symptoms to identify patterns. When do symptoms typically start? What early warning signs appear first? What strategies have helped in previous years? This information helps you and your healthcare providers fine-tune your treatment plan.
Safety Considerations and Finding Quality Treatment
While SAD treatments are generally safe, certain medical conditions require extra caution. If you have diabetes or eye diseases, get an ophthalmologic exam before starting light therapy. If you have bipolar disorder, light therapy could trigger a manic episode, so work closely with a psychiatrist. Some medications make you more sensitive to light, requiring adjusted protocols.
When selecting a light therapy device, look for products that specify 10,000 lux output at a comfortable sitting distance, provide UV filtration, and have been tested by reputable organizations. Be skeptical of products making extraordinary claims or those significantly cheaper than established brands.
The Future of SAD Treatment
Research continues to advance our understanding and treatment of SAD. Scientists are exploring personalized therapies based on genetic profiles, optimal combinations of light wavelengths, and new medications targeting specific brain circuits. Digital health tools, from apps delivering CBT techniques to smart light systems that adapt to individual circadian rhythms, show promise for making treatment more accessible and effective.
However, experts caution against unproven treatments. Products like light-emitting earplugs or dawn simulation glasses might sound innovative, but they lack scientific validation. Stick with evidence-based treatments while keeping an eye on emerging research.
Working With Winter Rather Than Against It
One of the most counterintuitive insights from winter mindset research is that acceptance and adaptation may be more effective than resistance. This doesn’t mean passively accepting depression or dismissing genuine symptoms. Instead, it involves distinguishing between what requires clinical treatment and what requires behavioral adjustment.
Attention as a Tool
Winter, like most complex experiences, contains both challenges and opportunities. What we choose to focus on significantly influences our emotional response. A cold, rainy day can be framed as making commutes difficult and outdoor activities unpleasant, or as perfect weather for reading, creative projects, cooking elaborate meals, or other indoor pursuits that summer’s demands often crowd out.
This intentional attention shift isn’t about toxic positivity or denying difficulties. It’s about a balanced perspective, acknowledging challenges while actively noticing and engaging with winter’s genuine offerings. Research demonstrates that this attentional focus significantly affects motivation, behavior, and, ultimately, mood.
Seasonal Permission
Modern culture often emphasizes year-round consistency in productivity, socializing, and activity levels. This expectation conflicts with natural biological rhythms and sets people up for feelings of failure or inadequacy when winter naturally slows their pace.
Granting yourself explicit permission to operate differently in winter, sleeping more, socializing less frequently, pursuing quieter activities, and reducing non-essential commitments can transform the season from a period of struggling against natural tendencies to one of intentional restoration. This practice of seasonal adaptation may also prepare individuals for other life periods that require slowing down, such as illness, major life transitions, or grief.
Winter-Specific Pleasures
Rather than merely tolerating winter until spring arrives, actively cultivating winter-specific pleasures creates anticipation and engagement with the season. This might include starting winter reading lists, planning indoor hobbies, establishing cozy evening routines, or exploring winter recreation like skiing or ice skating.
The goal is identifying activities that are genuinely better in winter, things that summer’s pull toward outdoor activities might otherwise displace. Whether that’s baking projects, craft work, catching up on films, or simply enjoying candlelit dinners, these intentional seasonal pleasures provide both structure and genuine sources of enjoyment.
If you’re struggling with winter depression, remember there’s no need to suffer in silence. Reach out to a healthcare provider, try evidence-based treatments, and give yourself permission to need extra support during challenging months. Spring will come, but you don’t have to white-knuckle it through winter anymore. With proper treatment and support, you can find your own light in the darkness.
How A Psychologist Can Help
As a clinical psychologist, I can help you identify problem areas and develop an action plan to change them. We are uniquely trained to understand the connection between the mind and body. I can offer strategies to adjust your goals so that they are attainable, as well as help you change unhealthy behaviors and address emotional issues. In my practice, I use a variety of evidence-based treatments to help people improve their lives. You are cordially invited to call my office at 844-802-6512 or to schedule an appointment online.
Frequently Asked Questions About Seasonal Affective Disorder
What is Seasonal Affective Disorder (SAD)?
Seasonal Affective Disorder is a type of depression that follows a seasonal pattern, most often beginning in fall or winter and improving in spring. It is linked to reduced daylight, circadian rhythm disruption, and changes in serotonin and melatonin.
What is the difference between winter blues and Seasonal Affective Disorder?
The winter blues are mild and temporary mood changes that do not disrupt daily life. Seasonal Affective Disorder is more severe, lasts weeks to months, and significantly affects mood, energy, sleep, and functioning. SAD is a diagnosable condition that requires treatment.
What are the most common symptoms of Seasonal Affective Disorder?
Common symptoms include persistent low mood, fatigue, increased sleep, carbohydrate cravings, difficulty concentrating, social withdrawal, and loss of interest in activities. Symptoms return around the same time each year and improve with treatment.
What causes Seasonal Affective Disorder?
Seasonal Affective Disorder is caused by reduced exposure to daylight, which disrupts circadian rhythms and affects serotonin and melatonin levels. Genetic vulnerability and reduced sensitivity to light also contribute.
How common is Seasonal Affective Disorder?
About 5 to 6 percent of Americans, roughly 10 million people, meet the criteria for Seasonal Affective Disorder. An additional one-third of adults experience milder seasonal mood changes.
What treatments work best for Seasonal Affective Disorder?
The most effective treatments include light therapy using a 10,000-lux light box, Cognitive Behavioral Therapy for SAD (CBT-SAD), antidepressant medication when indicated, and lifestyle strategies such as regular exercise and daylight exposure.
How does light therapy help Seasonal Affective Disorder?
Light therapy helps reset the body’s circadian rhythm and increases serotonin activity. Morning exposure to bright light can reduce fatigue, improve mood, and relieve other SAD symptoms in many people.
Can therapy help with Seasonal Affective Disorder?
Yes. CBT-SAD helps change negative thought patterns about winter and increase helpful behaviors. It has been shown to reduce symptoms and lower the risk of SAD returning in future years.
When should someone seek help for winter depression?
Professional help is recommended if symptoms last more than two weeks, interfere with daily life, or include persistent sadness, withdrawal, or sleep and appetite changes.
Is Seasonal Affective Disorder a type of depression?
Yes. Seasonal Affective Disorder is a form of major depressive disorder with a seasonal pattern. It shares the same core features of depression, including persistent low mood and loss of interest, but follows a predictable seasonal cycle.
How is Seasonal Affective Disorder different from other forms of depression?
Unlike non-seasonal depression, SAD is closely linked to reduced daylight and circadian rhythm disruption. Symptoms typically begin in the fall or winter and improve in the spring, while other depressive disorders may occur year-round.
What is the difference between winter blues and depression?
The winter blues involve mild, temporary mood changes that do not impair daily functioning. Depression, including Seasonal Affective Disorder, causes persistent symptoms that interfere with work, relationships, sleep, and overall quality of life.
What symptoms overlap between Seasonal Affective Disorder and depression?
Both SAD and other depressive disorders can include low mood, fatigue, reduced motivation, difficulty concentrating, sleep changes, and withdrawal from activities. SAD often includes increased sleep and carbohydrate cravings.
What causes depression to worsen in winter for some people?
Reduced daylight disrupts circadian rhythms and affects the regulation of serotonin and melatonin. For individuals biologically sensitive to light changes, these disruptions can trigger or worsen depressive symptoms during winter months.
How common is Seasonal Affective Disorder compared to depression overall?
About 5 to 6 percent of Americans experience Seasonal Affective Disorder. Many more experience seasonal worsening of an existing depressive disorder, even if they do not meet full criteria for SAD.
Can Seasonal Affective Disorder occur with other mental health conditions?
Yes. SAD commonly co-occurs with major depressive disorder, anxiety disorders, ADHD, and bipolar disorder. Co-occurring conditions may affect treatment choices and should be evaluated by a mental health professional.
Are treatments for Seasonal Affective Disorder different from depression treatment?
SAD treatment includes standard depression therapies such as psychotherapy and medication, with the addition of targeted interventions like light therapy and circadian rhythm regulation.
Does therapy help both Seasonal Affective Disorder and depression?
Yes. Cognitive Behavioral Therapy, including CBT-SAD, is effective for treating both seasonal and non-seasonal depression by addressing thought patterns, behaviors, and emotional regulation.
When should someone seek help for seasonal or winter depression?
Help is recommended when symptoms last longer than two weeks, recur each winter, or interfere with daily functioning. Early treatment improves outcomes for both SAD and other depressive disorders.
Can Seasonal Affective Disorder turn into major depression?
Seasonal Affective Disorder is already classified as a form of major depression. Without treatment, symptoms may worsen over time or overlap with non-seasonal depressive episodes.
How does a psychologist help with depression that worsens in winter?
A psychologist can assess whether symptoms reflect SAD, major depression, or both, and develop a personalized treatment plan using evidence-based approaches such as CBT, behavioral activation, and light therapy guidance.
People Also Ask
Is Seasonal Affective Disorder real?
Yes. SAD is a recognized form of major depression with a seasonal pattern.
How long does Seasonal Affective Disorder last?
Symptoms usually begin in the fall or winter and improve in the spring.
Can vitamin D help Seasonal Affective Disorder?
Vitamin D may help some people, especially those who are deficient.
Is light therapy safe for SAD?
Light therapy is generally safe but should be used under professional guidance for specific medical conditions.
Can SAD come back every year?
Yes. SAD often follows a predictable yearly pattern without treatment.
Is SAD more common in women?
Yes. Women are affected about four times more often than men.
Can Seasonal Affective Disorder be prevented?
Starting treatment early in the fall can reduce or prevent symptoms.